Sleep is a complex biological process. While we are sleeping, we are unconscious, but our brain and body functions are still active. Sleep is generally divided into 4 stages. The stages are termed as Stage N1, Stage N2, Stage N3 and Rapid Eye Movement (REM) Sleep Stage. Good sleep is necessary for optimal health and can affect hormone levels, mood and weight.
Sleep disorders comprise a variety of conditions ranging from insomnia (inability to sleep) to conditions related to hypersomnia (the inability to remain awake). Therefore as previous research has shown, it is detrimental to one’s health to either sleep too much or to sleep too little.
Among the various sleep disorders, Sleep Related Breathing Disorder is an entity which carries significant detrimental effects to the individual who suffers from it. Sleep Related Breathing Disorders are characterized by disordered respiration during sleep. It comprises three entities and they are Obstructive Sleep Apnea, Central Sleep Apnea (CSA) and Sleep Related Hypoventilation Syndromes.
What Is Obstructive Sleep Apnea?
Obstructive Sleep Apnea (OSA) is the most common Sleep Related Breathing Disorder. It is the most important and common sleep disorder affecting the global community. It is no different in our country, Malaysia although it is still largely under recognized and under diagnosed. Malaysia ranks as the country with the highest rate for obesity in South East Asia. Furthermore it is no hidden secret that obesity is one of the main causes that result in Obstructive Sleep Apnea. Nevertheless, there have been many researches which have shown that due to our (Asian) facial profile, we Asians are at higher risk to develop Obstructive Sleep Apnea even at lower weights compared to Caucasians.
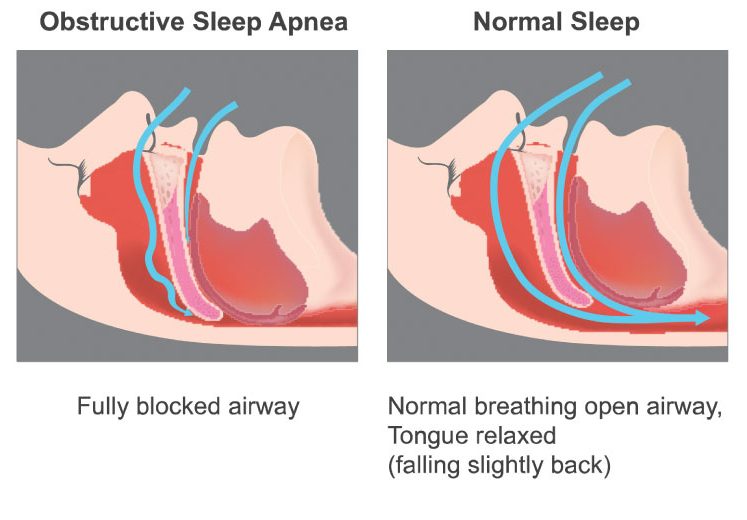
The hallmark feature of Obstructive Sleep Apnea are recurrent episodes of partial (hypopnea) or total collapse or closure (apnea) of the upper airway during sleep. This leads to repeated episodes where there is lack of oxygen reaching the vital organs during these apneic episodes and also failure to expel carbon dioxide from the body.

Who Is At Risk Of Having Obstructive Sleep Apnea?
There are many factors which contribute to the development of OSA. The size of the upper airway which is smaller in certain ethnic groups make them more predisposed to develop this condition. An individual who is obese has a higher risk of developing OSA due to excess fat tissue around the airways which makes it narrower to start with, which in turn increase the risk of closure during sleep. In a normal physiological response during sleep, the upper airway muscles tend to relax. However in patients with OSA, the degree in which the muscles relax tends to be greater and as a result the airways have a higher tendency to collapse. Risk factors for the presence of OSA include obesity, being of male gender, older age, and postmenopausal status (not on Hormone Replacement Therapy). There has also been evidence to show that severe OSA has a higher prevalence in Asian and Latin Americans at a much lower BMI compared to their Caucasian counterparts. Multiple clinical studies have been conducted on this aspect and they have attributed this phenomenon to the smaller airways sizes and the different craniofacial profile in these ethnic groups.
Are Women Protected From Obstructive Sleep Apnea?
Sleep-disordered breathing has been assumed to be a condition associated predominantly with men. Community-based studies have shown that the male to female ratio for OSA is in the range of 2:1 or 3:1. In the epidemiological study by Young et al. it was estimated that 2% of adult women and 4% of adult men fulfilled diagnostic criteria of OSA. The possible mechanisms underlying the differences in the prevalence of OSA in men and women are not fully understood. Gender differences in the structure and physiological behaviour of the upper airway, including craniofacial morphology, and the pattern of fat deposition have been proposed to account for a higher predisposition for males to develop OSA. However there is increasing data that suggest the prevalence of OSA in females is actually higher than what traditional literatures predict. It is likely that women with OSA are under-diagnosed due to circumstances related to their role in the family and social lifestyle. The influence of a different clinical expression of OSA in women might also contribute to difficulties in initially suspecting this disorder. Women tend to present more with insomnia and depression rather than the traditional symptoms of snoring and daytime sleepiness. Furthermore women tend to be less forthcoming in admitting to snoring.
How Do You Suspect That You May Have Obstructive Sleep Apnea?
As a result of the apneic episodes, patients with OSA tend to manifest symptoms which may be categorized as daytime and nocturnal symptoms. The presence of these symptoms can alert the individual to the possibility of having OSA and thus motivate them to seek professional help. Important nocturnal symptoms can be identified by asking the spouse or bed partner of the individual. Among the most common symptoms highlighted by the bed partners are loud snoring, nocturnal choking and episodes where the bed partners observe that the individual stops breathing during sleep. This is usually described by the spouse as “I wake up in the middle of night and notice that my spouse is not breathing, unsure whether he is alive, and then suddenly he gasps for air and then the snoring starts again. This cycle repeats throughout the night.
Other nocturnal symptoms are frequent arousal during the night with poor quality of sleep. Patients also experience frequent episodes of passing urine at night (nocturia).
Patients also present with daytime symptoms such as early morning headaches, sleep that is not refreshing, poor concentration during daytime activities, irritability and daytime sleepiness. These symptoms can be assessed by a Sleep Physician during their interview with the patient. Certain tools such as the Epworth Sleepiness Scale can be used to assess the degree of daytime sleepiness. Another important symptom is falling asleep while driving which can be a wake up call for an individual to seek professional consultation.

How Do I Confirm I Have OSA?
To confirm the presence of OSA, the individual has to undergo a diagnostic test which is commonly known as a Sleep Study which will be able to document the frequency of breath pauses and decreased oxygenation, and thus grade the severity of the OSA. It is paramount that the individual with symptoms of sleep disturbances consult a qualified Sleep Medicine Physician before embarking on any tests. This is to allow the doctor to differentiate and diagnose the sleep disorder experienced by the individual. Not all sleep disorders require a sleep study to be diagnosed. Some sleep disorders require other forms of diagnostic studies such as a Multiple Sleep Latency Test which is used to diagnose Narcolepsy. Furthermore, even if an individual requires a Sleep Study, the Sleep Medicine Physician will be able to decide whether a Full Sleep Study or a Portable Sleep Study is warranted.

What Is The Importance Of Diagnosing And Treating OSA?
The importance of recognizing and treating OSA rests in the fact that the presence of untreated OSA increases your risk of heart problems and strokes. Among the heart problems which are related to OSA includes heart failure, early heart attacks, abnormal heart rhythm (cardiac arrhythmias) and sudden cardiac deaths. The prevalence of OSA in patients with Heart Failure can reach up to 76%.
The risk factors for patients with OSA to have heart failure:
-
-
- in males, a body mass index (BMI) of more than 35.
- in females, being at the age of more than 60 years old.
-
Patients with OSA have a higher incidence of hypertension. The prevalence of OSA in patients with hypertension ranges about 40-60%. In patients with drug resistant hypertension the prevalence of OSA has been documented to be up to 83%. Making OSA one of the most under-recognized causes of secondary hypertension. Among patients who have abnormal heart rhythms which require pacemaker insertions, the prevalence of OSA can reach up to 59% as shown in certain publications. OSA might be a risk factor for heart attacks or angina pectoris (chest pain related to blockage of blood vessels supplying the heart), and middle-aged men might be at a higher risk.
A number of studies have shown a high prevalence of sleep- related breathing disorders in patients soon after a stroke. In a study conducted in 2003, patients who were treated for OSA with positive airway devices showed a 37% reduction in risk of heart disease and a 56% reduction in risk of stroke. Besides increasing the risk of stroke, the presence of untreated OSA also plays a part in causing neurocognitive function deterioration in these patients. Patients with untreated OSA tend to have an adverse effect on inductive and deductive reasoning, attention, vigilance, learning, and memory.
The presence of OSA in patients with diabetes is about 50%. Patients with untreated OSA have been shown to have poorer sugar readings and poorer diabetes control. Males with untreated OSA also tend to be at higher risk of developing erectile dysfunction especially in those with severe OSA. With proper treatment of their underlying OSA, studies have shown improvement in the erectile function. Depression is also higher in patients with untreated OSA. Therefore, looking at the immense effect untreated OSA has on the health of an individual, it is still a wonder why this disease is still under-recognized by both doctors and patients.

Is OSA Treatable?
The treatment of OSA requires a multi-disciplinary approach. As the disease is a result of multiple factors such as obesity, airway anatomy and excessive relaxation of upper airway muscles which result in airway collapse, the condition cannot be treated with only addressing a single aspect of the predisposing condition. The ultimate aim of treatment is to maintain the airway during sleep, thereby ensuring adequate oxygenation throughout the night. This can be accomplished by using a device which provides positive airway pressure at night which allows the airway to remain open during sleep.
This device is called a Positive Airway Pressure (PAP) device and it has been shown to be highly effective. Of course other issues also need to be addressed such as weight reduction and upper airway anatomical problems. But the gold standard of treatment worldwide are PAP devices. Weight reduction can help to reduce the pressure needed to maintain the upper airway patent. Weight reduction can be achieved by diet and exercise and the amount of weight reduction has to be significant to have an impact on OSA. But of course in reality most studies have shown that it is usually difficult to maintain weight loss. Another approach to consider is bariatric surgery. Surgery for upper airway anatomy was something which was done about 20 years ago to treat OSA. But current evidence places these upper airway surgeries more in the role of a complimentary surgery to help increase compliance to the Positive Airway Pressure devices.
The main problem with PAP devices is for the patients to be compliant to these devices which require a period of acclimatization to the devices and lifestyle modifications as present in treating any other disease. Furthermore it is not about just sending the patient home with the PAP device. This is where the role of Sleep Medicine Physician is important in personalizing the treatment for the individual. As OSA is a chronic disorder, the treatment is dynamic and requires fine tuning as the affected individual’s profile changes as he ages. Nevertheless, there have been other forms of treatment that have been put forward throughout the years. Among those are Maxillary advancement devices which have been offered as an option of treatment for patients who are unable to tolerate PAP devices. However, studies have shown that they are less effective when compared with PAP devices.
In conclusion, it is clear that OSA is a serious disorder which carries severe consequences to the individual suffering from it. It has a multi-organ effect and requires a systematic and multi-disciplinary approach to overcome it.
 Dr Muventhiran Ruthranesan
Dr Muventhiran Ruthranesan
Consultant Respiratory, Internal Medicine and Sleep Medicine, Pantai Hospital Ayer Keroh


