In 2019 alone, heart (cardiovascular) disease claimed an estimated 18.6 million lives (a staggering figure you can’t wrap your head around!) across the world, according to the World Heart Federation, with Malaysia accounting for 18,267 in total.
As we celebrate World Heart Day on 29 September, Dr Azani Mohamed Daud, Cardiologist – Gleneagles Hospital Kuala Lumpur imparts a wealth of invaluable insight on heart disease, Malaysia’s No 1 killer, with hopes of magnifying the gravity of the disease, its risk factors and prevention.
Living a long, healthy, happy, contented life is what dreams are made of for every single one of us – the haves, the have-nots, regardless of social status, creed, religion. Chances are, though, the majority of us have experienced, at some point in our lives, the anguish and pain of losing a loved one, or at least know of someone who has. And it wouldn’t be a stretch at all to point the finger in the direction of ‘heart disease’ as the damning culprit.
According to the ‘Statistics on Causes of Death, Malaysia’ report issued last November by Department of Statistics Malaysia, the deviously stealthy heart disease remains Malaysia’s No 1 killer, increasing from 13.2% of all medically certified deaths in 2016 to 17% in 2020, which translates to a total of 18,515 deaths.

Heart (cardiovascular) disease is still the No 1 killer in Malaysia. What are your thoughts on this?
Yes, cardiovascular (CV) disease has been the No 1 killer in Malaysia for many years. At the height of the Covid-19 pandemic, death rates from Covid-19 were extremely high too and it is possible that Covid-19 deaths may have superseded documented CV deaths, but we need to wait for the statistics for those years to be released. Whatever the case may be, CV death rates remain far too high in Malaysia.
What are the risk factors of heart disease?
Essentially there are two types of risk factors – modifiable and non-modifiable. The non-modifiable risk factors are family history (where genetics strongly influences CV risk), age (the risk of a CV event increases with age), and gender; everything else being equal, males have a higher risk compared to females.
Some of the modifiable risk factors are smoking, hypertension (most people with high blood pressure do not experience any symptoms, hence hypertension is known as the ‘Silent Killer’), diabetes and elevated levels of LDL-cholesterol (‘bad cholesterol’). Obesity is another risk factor. Unfortunately, a very high proportion of the Malaysian population is overweight or obese; in fact, Malaysia ranks as the worst amongst ASEAN countries. Obesity is associated with CV diseases, pre-diabetes and diabetes, hypertension, certain cancers and joint problems, among others.
Sedentary lifestyles also contribute to obesity, so it’s recommended that we exercise about 150 minutes a week. Regular exercise also reduces risk of pre-diabetes and diabetes, and lowers blood pressure. A lot of my patients cite a lack of time as the main reason for not exercising and I usually advise them to incorporate physical activity into their daily routine. For example, instead of using the elevator, walk up the stairs… instead of driving to nearby shops or places of worship, walk there instead.
Stress is also another modifiable risk factor. Levels of stress hormones may increase during periods of stress; amongst these are adrenaline which causes an increase in heart rate and blood pressure as well as cortisol which increases blood sugar levels.
What are the common causes of heart problems among Malaysians?
It would be wrong to pin the reason down on just one factor. I believe that overall lifestyle plays a significant role including all the modifiable risk factors listed above. Late-night eating at warungs is just an example of a less healthy lifestyle. Raiding the fridge late at night to snack on leftovers or ice-cream is probably not much different!
What are the signs and symptoms to look out for?
To understand possible signs and symptoms of coronary heart disease, it’s perhaps better to first understand the underlying disease process.
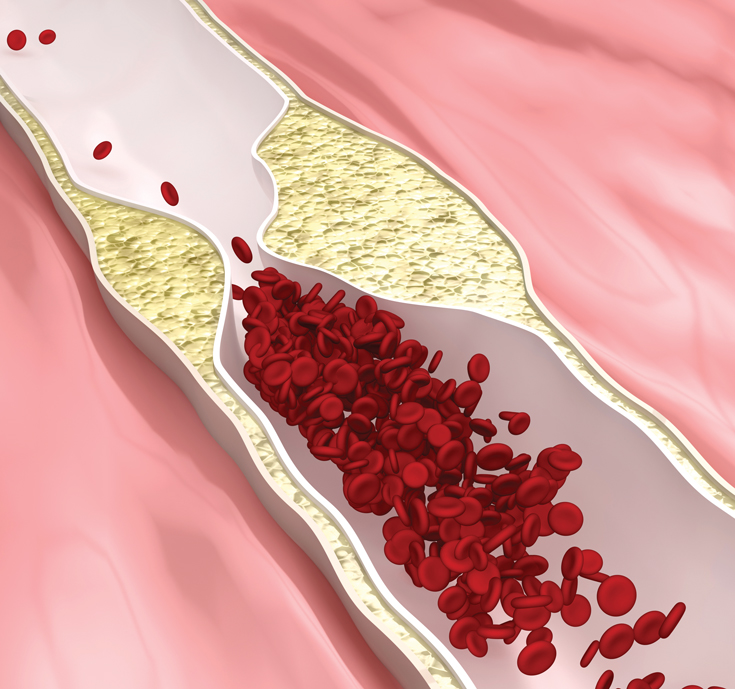
The fundamental problem is the formation of cholesterol deposits (plaques) within blood vessels. This process takes place in all the blood vessels of the body including those supplying the heart, brain, kidneys and limbs, to name a few. There are two important effects that can arise from this process; the first is the narrowing of the blood vessel resulting in a reduction in blood flow to the organ supplied by the said vessel, also known as stenosis of the blood vessel. This process is slow and takes place over many years but is accelerated by the risk factors discussed above, especially diabetes and high LDL-C levels. If we look at the heart, should the blood vessels become significantly narrowed, the flow of blood may be impeded enough to affect the supply of oxygen to the heart especially when the heart is beating fast and oxygen demand increases. This imbalance in oxygen supply and demand to the heart tissue can result in symptoms such as chest discomfort. Typically the chest discomfort occurs in the centre of the chest although it may be anywhere in the chest and may extend into the neck, jaw and arms. The discomfort occurs when the heart rate increases, for example during physical activity, and subsides as the heart rate slows down with rest. It may also be associated with sweating and shortness of breath. Typically, symptoms occur when there is a narrowing of at least 60-70%. It is possible to have more than one area of narrowing in a blood vessel.
The second effect is rupture of a cholesterol plaque, which occurs after a plaque becomes inflamed. This rupture causes the immediate formation of a blood clot within the blood vessel at the site of the rupture, leading to an absolute cessation of blood flow. The tissues supplied by the affected blood vessel downstream to the clot will receive no blood supply and the tissue dies. If this occurs in a vessel supplying the heart, it will result in a HEART ATTACK.
The symptoms of a heart attack typically include severe chest pains, profuse sweating, vomiting and shortness of breath. The damage to the heart tissues can also trigger off an abnormal heart rhythm which can lead to a cardiac arrest and death. Unfortunately for some people, the first symptom they experience is a heart attack leading to cardiac arrest and death immediately.
What are the tests/screenings available to check for heart disease?
There are a number of tests available mostly to look for narrowings of the coronary arteries, less so for the risk of rupture. The types of test depend on the CV risk of an individual patient. There really is no ‘one size fits all’.
Amongst the list of available tests for the heart are electrocardiogram (ECG), echocardiogram (an ultrasound scan of the heart), treadmill exercise stress test, coronary calcium score, cardiac MRI scan (including perfusion studies), CT angiogram of the coronary arteries, and coronary angiogram.
What are the treatment options?
The treatment options generally depend on the extent of the disease. If there are significant narrowings in the coronary arteries detected following investigations, the options for treatment include Optimal Medical Therapy (OMT), the use of drugs in optimal, maximally tolerated doses to offset the effects of narrowings on blood flow in the vessels supplying the heart; Percutaneous Coronary Intervention (PCI), a non-surgical procedure using balloons with or without the use of stents to re-open the narrowings in the blood vessels; and Coronary Artery Bypass Graft (CABG) surgery, an open-heart surgery where blood vessels in the chest or legs are harvested and used to create a diversion bypassing the narrowings and implanted into the non-narrowed segments of the heart blood vessels to improve flow.
In the event of a heart attack, time is of the essence. The best way of treating a heart attack is to perform emergency PCI and re-open the affected blood vessel and restore blood flow. Results are best if PCI is performed within an hour of the heart attack occurring, the sooner the better. In hospitals where such facilities are not available, clot-buster drugs can be given to dissolve the blood clot and restore flow.
What steps should we take to prevent heart disease?
The most important step is to optimally control all the modifiable risk factors and lead an all-encompassing healthy lifestyle. Quit smoking, eat moderately and exercise regularly. It’s important to see your doctor to have your blood pressure and cholesterol levels checked, as well as glucose levels to detect not only diabetes but also pre-diabetes.
Remember, it’s very possible to have elevated blood pressure, glucose and cholesterol levels as well as cholesterol deposits in the blood vessels, and yet display absolutely no symptoms. All it takes is for one of the deposits to rupture, induce a heart attack and cause a cardiac arrest and death.

Source of Statistics:
- Department of Statistics Malaysia www.dosm.gov.my
- World Heart Federation www.world-heart-federation.org
 Dr Azani Mohamed Daud
Dr Azani Mohamed Daud
Cardiologist,
Gleneagles Hospital Kuala Lumpur.


