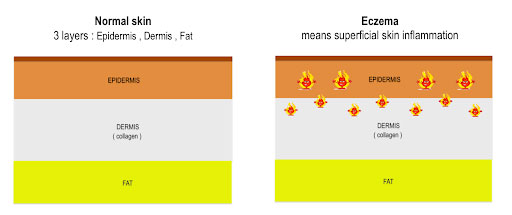
What is eczema? Eczema simply means inflammation of the outer layer of our skin. When harmless irritants or allergens outside our body “switch on” the overactive immune system, it produces uncontrolled eczema. It can be likened to “setting the skin on fire”. Controlled inflammation is a natural defense mechanism of our body.
Inflammation plays a central role in fighting infection and in the healing process, but left to run wild, this process can lead to various forms of eczema. BabyTalk had a chat about this topic with Dr Leong Kin Fon, a Consultant Paediatric Dermatologist fromHospital Kuala Lumpur (HKL), and here’s what we discovered.
NH: How many types of eczema are there ?
Dr Leong: Eczema is often used as a blanket term describing various forms of specific rashes due to superficial skin inflammation. Various forms of eczema include :
1. Atopic eczema
2. Contact eczema
3. Dyshidrotic eczema
4. Discoid eczema
5. Seborrheic eczema
6. Others: statis eczema, asteatotic eczema
It is not uncommon to have more than one form of eczema on your body at the same time. Each form of eczema has its own set of triggers, predisposing factors , clinical appearance, natural course and treatment strategies.
NH: What are the common symptoms of Atopic Dermatitis (AD)?
Dr Leong: Itchiness is the main feature of eczema. Eczema is sometimes referred to as “the itch that rashes” because the itching usually comes first. In the absence of characteristic redness among the dark-skinned, skin itchiness and scaliness may help patients in early detection of eczema flare-up.
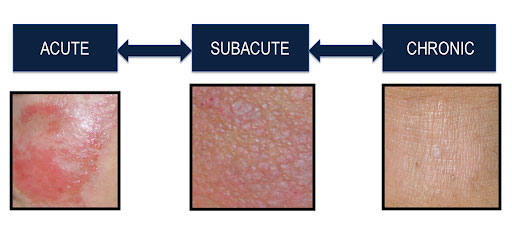
Clinically, eczema has many faces of presentation that vary with its
A. Chronicity
During acute stage : dry, scaly, redness, blister, erosion
During chronic stage : thickened, discolored and leather like texture
B. Background skin color
It can present differently in different skin colors.
Among the light-skinned, eczema appears as scaly red
However, in brown or dark-skinned, eczema rashes are less visible. It tends to look ashen grey, brown, or purple among dark skinned.
BT: What is the root cause of atopic eczema ?
Dr Leong: Atopic eczema is a multifactorial inflammatory skin disorder. It is due to dynamic interaction between multiple genetic and environmental factors. The mathematic of atopic eczema is Atopic eczema = Genetic + Environment irritants + Environmental allergens + overgrowth of skin bacteria
Environmental factors include:
- Sweat related to hot and humid weather
- Prolonged and frequent exposure to chlorinated swimming pool
- Friction related to tight clothing and shoes
- Itch scratch cycle
- Harsh cleanser or creams
- Imbalance between friendly & harmful bacteria i.e. overpopulated by Staphylococcus aureus
- Others : food allergens, aeroallergens, stress
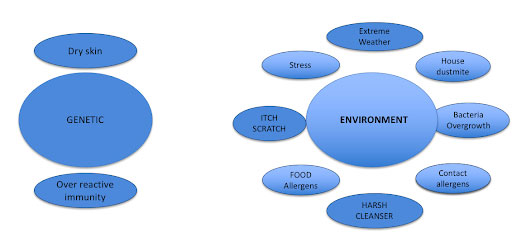
NH: Why do some children have AD?
Dr. Leong: Atopy refers to the genetic tendency to asthma, eczema and hay fever. Genetics play a “significant but not absolute” role in determining who will get eczema. Despite the genetic background, some children with family history of atopy never develop atopic eczema. On the other hand, children from a non-atopic family can suffer from it due to harsh environmental factors, i.e. urbanization. Hence, familial aggregation is due to shared environment and / or shared genes.
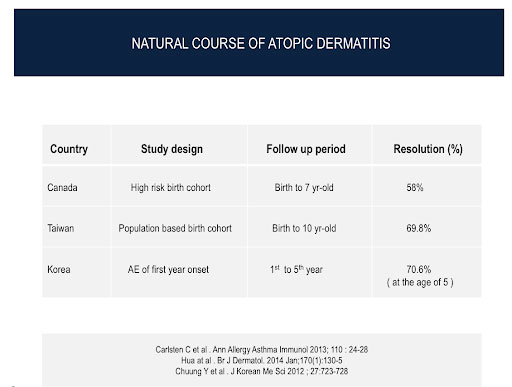
BT: Will children grow out of eczema?
Dr. Leong: Most children affected by early onset atopic eczema will see significant improvement (outgrow) as they get older. However, the majority continue to have variable degrees of dry skin and at higher risk of allergic or irritant contact eczema. Therefore , lifelong avoidance of harsh irritants such as soaps, detergents and bubble baths is beneficial. Although atopic eczema cannot be cured, there are many ways of controlling it and many promising medications are in the pipeline.
NH: Is it true there is a seven-year cycle?
Dr. Leong: Not true
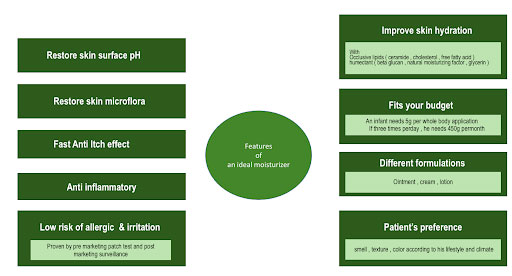
NH: Why are emollients (moisturisers) so important and what type of moisturiser should one choose for a child?
Dr. Leong: Dry skin is very common among atopic eczema patients. It is one of the key components that present in all stages of eczema.
Moisturisers are the mainstay of treatment for atopic eczema and regular application has anti itch and steroid sparing effect.
Rules about moisturiser application in atopic eczema
- Moisturiser should be applied regularly and liberally
- Moisturiser should be applied to the entire body immediately after bath or whenever they feel dry and itchy.
- Moisturiser should be coupled with a gentle cleanser
- Moisturiser should be continued even when the eczema has cleared
- Moisturiser should be provided in different formulations and patients should be encouraged to select the regimen that will best meet their lifestyle and weather. Ointments may be preferred for night time use because of their longer lasting hydrating properties. But ointment based moisturisers can be uncomfortable and sticky in hot weather.
NH: With the current pandemic, does using hand sanitiser or frequent hand-washes affect the condition?
Dr. Leong: Yes, hand eczema is more common during the Covid-19 pandemic due to the irritation and drying effect of excessive usage of sanitiser and frequent hand washing.
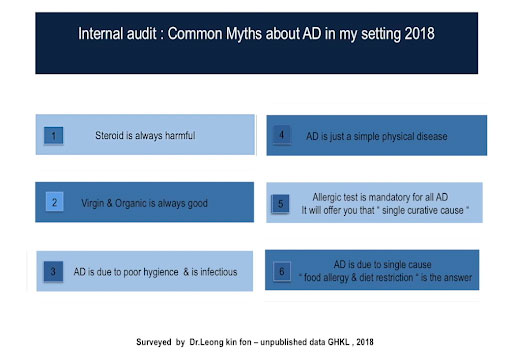
NH: What are the common misconceptions about AD and mistakes made in managing the condition? How can we improve?
DR. Leong: Active listening , organized education programmes and empowerment are the antidote to myths and fallacies about atopic eczema.
The common misconceptions about atopic eczema are as below :
- Steroid cream is always harmful
- Atopic eczema is due to food allergy and diet restriction is the first line of treatment
- Organic and virgin creams are always effective and safe
- Allergy tests are mandatory for all children with atopic eczema for diagnosis and underlying cause
- Atopic eczema is due to poor hygiene
- Atopic eczema is self-limiting and we should let the disease run its course. Active treatment is not needed
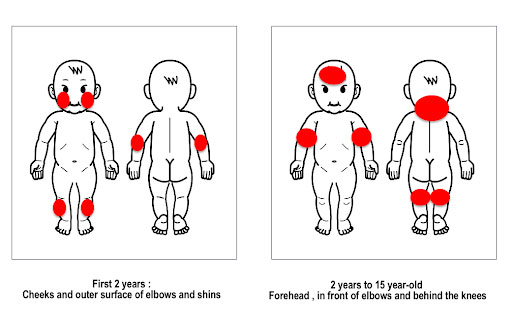
NH: Is AD a static condition, does it change throughout our life cycle?
Dr. Leong: No, AD is a dynamic inflammatory skin disorder. Firstly, the pattern of atopic eczema varies with their age group
Secondly, the appearance of atopic eczema gets darker, thickened and leather like texture over years. It is important to treat early eczema as chronic lichenified eczema is less responsive to treatment.
NH: Can children (in their teens) be vaccinated if they suffer from AD?
Dr. Leong: Yes, all children with atopic eczema should be vaccinated according to the national vaccination program. But vaccination should be delayed during an eczema flare up until his eczema is stabilized when a patient is on systemic treatment i.e. prednisolone, azathioprine , methotrexate etc.
Do check out our News & Events column for an outstanding product to help bring relief to eczema sufferers.
 Q & A with Dr Leong Kin Fon
Q & A with Dr Leong Kin Fon
Consultant Paediatric Dermatologist,
Hospital Kuala Lumpur (HKL)


