In many people’s minds, the image of the elderly is usually weak, fatigued, slow or lacking energy. They do not usually pay much attention to these symptoms. Sometimes the elderly themselves may feel unwell, but they should not be feeling helpless, as that is not part of normal ageing.
Frailty is a condition characterised by an increased risk of death or debility following exposure to an environmental stressor. In other words, there is a reduced ability to withstand illness, and there may also be loss of function. In layman terms, it can be called weak, delicate or fragile.
Although frailty is not a disease, frail elderly are particularly susceptible to disease, and their daily activities and cognitive functions deteriorate more quickly, which can easily lead to some undesirable consequences, such as confusion, falls, fractures, immobility, disability, malnutrition, polypharmacy (the use of five or more medications), increased healthcare cost, recurrent hospitalisation, institutionalisation, and even death. We need to understand though that not every older person will get frailty. More importantly, patients who are diagnosed with frailty will still have a chance of reversal.
The frailty check
Clinically, frailty is defined mainly based on the five characteristics proposed by Dr Fried in 2001, and it is also the most commonly used screening method at present. If a person (not only the elderly) meets 3 or more of the characteristics, they are considered frail, meeting 1 or 2 of the conditions is the pre-frail stage, and a score of 0 is considered a healthy elderly who is
not frail.
The Fried criteria include:
1) Unintentional significant weight loss: weight loss of more than 5 kg or 5% within 1 year.
2) Exhaustion: feeling tired for more than 3 days a week can predict disability and death.
3) Slow walking speed: walking less than 8 meters in 10 seconds can predict poor prognosis of disease treatment. For every 0.1 meter/ second increase in walking speed, the risk of frailty and death decreases by 12%.
4) Weakness / decreased muscle strength: impaired grip strength (less than 26 kg for men and 18 kg for women) can predict fatigue, disability, morbidity and mortality. Older people with poor grip strength are at higher risk of getting frailty by 6 times.
5) Low physical activity: men consume less than 383 calories a week, and women consume less than 270 calories a week.
Therefore, when the elderly in the family have poor appetite, weight loss, slower walking, fatigue and weakness, reduced self-care ability, reduction in the number of trips and activities, etc., you need to pay special attention, because these are all warning signs of frailty. In frailty, even mild diseases can lead to poor balance and become a risk factor for falling. In addition, delirium (confusion), repeated lung and urinary tract infections are also some of the signs of frailty in elderly people.
What causes frailty?
Frailty does not have one single cause, but many causes. Ageing, lack of exercise, insufficient nutrition, poor environment, trauma, diseases, and drugs can cause malnutrition and sarcopenia (syndrome characterised by progressive and generalised loss of skeletal muscle mass and strength), and frailty can also be caused by them. In terms of gender, the incidence of frailty in older women is higher than that of older men. Unmarried, divorced or widowed elders are at higher risk of frailty compared to married elders, because most of them live alone, have less contact with family and friends, and may have different degrees of isolation from society. There will be a certain sense of loneliness. Some mental diseases such as depression and dementia can also lead to frailty.
The older a person is, the higher the risk of frailty, because physical fitness and organs function decline with age. When young people fall sick, it is easier for them to return to a relatively healthy state, and this ability decreases with age.
In addition, disease is also one of the risk factors for frailty. Elderly people with chronic diseases have a higher risk of frailty than those without chronic diseases. Taking multiple drugs or even abuse of drugs will increase the risk of frailty. Of course, long-term bad habits, such as smoking, alcoholism, stress, sitting or staying in bed for a long time will also increase the risk of frailty.
Complications:
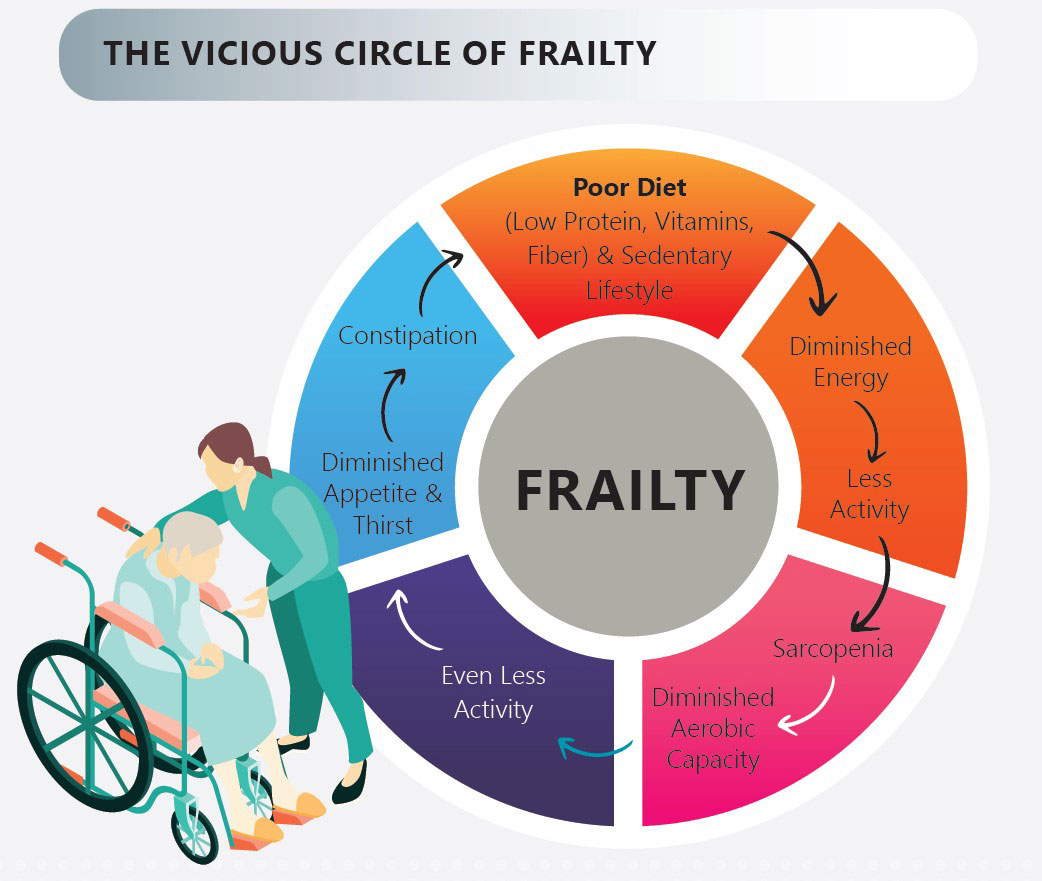
Malnutrition, sarcopenia and frailty affect each other, forming a vicious circle.
For example, malnutrition can lead to frailty, which will increase the risk of falls, and sarcopenia with reduced muscle strength. A significant decrease in muscle strength of the lower limbs will directly affect the balance and make it easier to fall. If falls and fractures cause immobility and reduced daily activities, the elderly may become weaker and lose muscle faster.
Frailty increases the risk of adverse events such as heart attacks and strokes, lung infections, confusion, and falls in the elderly. Physical frailty often leads to deterioration in cognitive ability and social participation. Once frailty occurs, the average risk of death increases by 15% to 50%.
It is not surprising to find that frailty is related to lower quality of life, higher risk of hospitalisation, and death. There will also be a need for long-term care of the elderly and an increase in medical expenses. The medical expenses and care expenses of those who are frail are almost twice that of the non-frail people. Therefore, early recognition of the symptoms of frailty in the elderly, timely diagnosis and intervention, will have the opportunity to reverse the frailty to the pre-frail or healthy state before the adverse outcome occurs.

Can frailty be prevented?
With the increase of the elderly population in our country and the extension of life expectancy, the problem of old age is also increasing day by day. It is estimated that frailty is present in one-tenth of the elderly over 65 years old, and up to half of those over 80 years old. The good news is that frailty can be reversed. Studies have shown that exercise and protein supplementation are the two key treatments, as well as the most effective and easiest preventive measures.
Exercise is the most effective way to improve the quality of life and function of the elderly. Appropriate physical activity can delay the progress of frailty. Therefore, we should encourage the elderly in the family to participate in diversified activities. Exercise should ideally be done 5 days a week at home, for about 20 to 25 minutes, including intensive training of arms and legs, and physical balance and coordination training. However, the intensity and duration of exercise should be determined according to the overall health of the individual, and the type of exercise can be based on individual interests. The forms of exercise can be diversified, such as walking, brisk walking, aerobics, dancing, Tai Chi, running, swimming, etc.
Nutritional intervention can improve the weight loss of malnourished and frail elderly people and reduce the mortality rate. The daily diet should include milk, eggs, meat and fish, as sufficient energy and protein can help maintain weight and muscle mass. As for Omega-3 fatty acids, it can improve appetite and weight. In addition, vitamin D supplementation can also improve the strength and function of the lower limbs.
For the elderly with poor appetite or those who are hospitalised, oral nutrition with high energy and protein content can improve their nutritional status.
In addition, the elderly often suffer from comorbidities such as hypertension and diabetes. Active management of the disease, especially focusing on reversible diseases, evaluating the rational use of medications, and stopping unnecessary medications, are effective in improving frailty.


