Your lungs are part of a complex system, expanding and relaxing thousands of times each day to bring in oxygen and send out carbon dioxide. Lung diseases can happen when there are problems in any part of this system.
Lung Diseases Affecting the Airways
Your windpipe (trachea) branches into tubes called bronchi, which in turn become smaller tubes throughout your lungs. Diseases that can affect these airways include:
- Asthma. Your airways are constantly inflamed and may spasm, causing wheezing and shortness of breath. Allergies, infections, or pollution can trigger asthma symptoms.
- Chronic obstructive pulmonary disease (COPD). With this lung condition, you cannot exhale the way you usually would, which causes trouble breathing.
- Chronic bronchitis. This form of COPD brings a long-term wet cough.
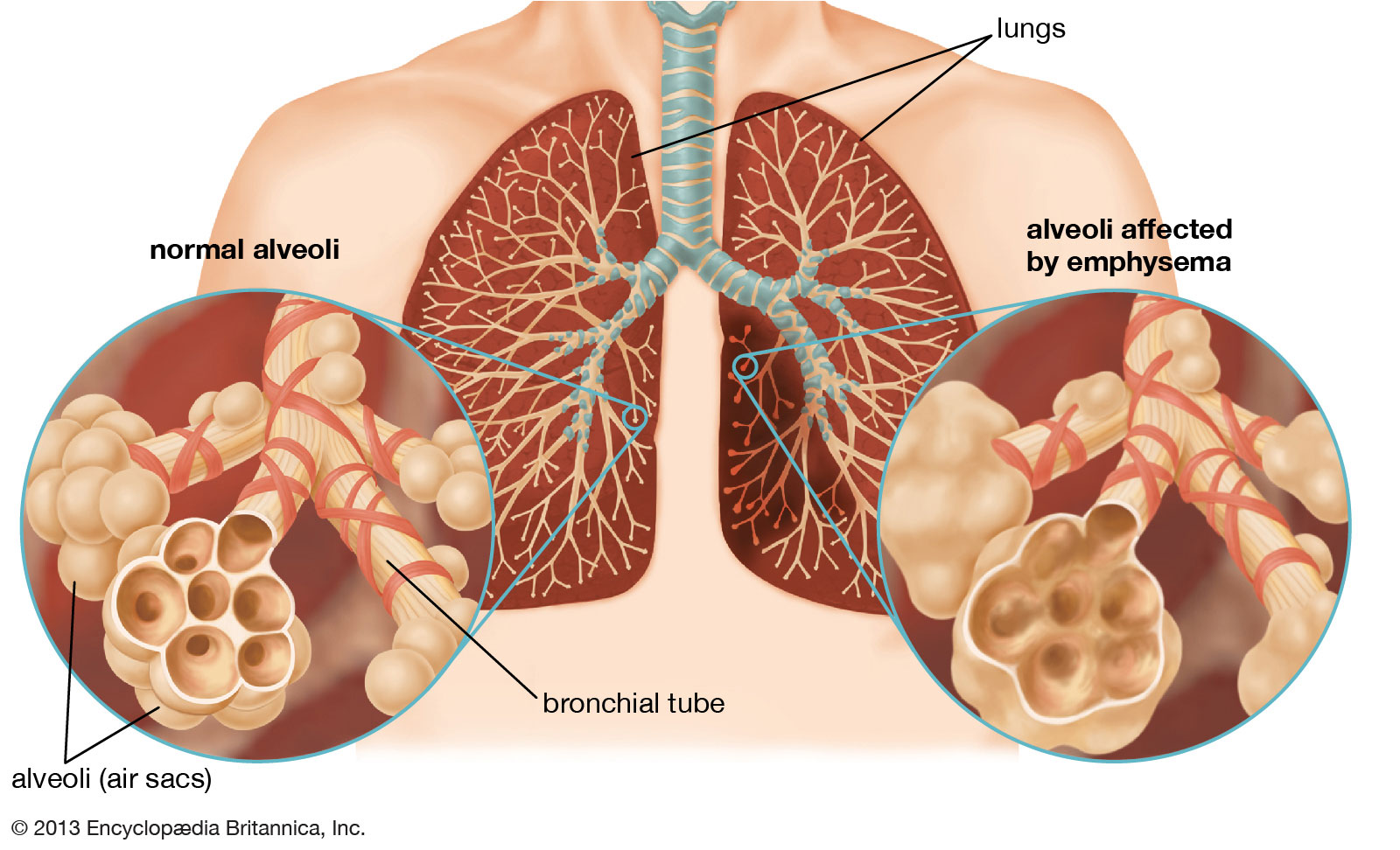
- Emphysema. Lung damage may cause trapped air in your lungs in this form of COPD. Trouble blowing air out is its hallmark.
- Acute bronchitis. This sudden infection of your airways is usually caused by a virus.
Lung Diseases Affecting the Air Sacs (Alveoli)
Your airways branch into tiny tubes (bronchioles) that end in clusters of air sacs called alveoli. These air sacs make up most of your lung tissue. Lung diseases affecting your alveoli include:
- Pneumonia. An infection of your alveoli, usually by bacteria or viruses, including the coronavirus that causes Covid-19.
- Tuberculosis. Pneumonia that slowly gets worse, caused by the bacteria Mycobacterium tuberculosis.
- Emphysema. This condition happens when the fragile links between alveoli are damaged. Smoking is the usual cause. (Emphysema also limits airflow, affecting your airways).
- Pulmonary edema. Fluid leaks out of the small blood vessels of your lungs into the air sacs and the area around them. One form is caused by heart failure and back pressure in your lungs’ blood vessels. In another form, injury to your lung causes the leak of fluid.
- Lung cancer. It has many forms and may start in any part of your lungs. It most often happens in the main part of your lung, in or near the air sacs.
Lung Diseases Affecting Blood Vessels
The right side of your heart gets low-oxygen blood from your veins. It pumps blood into your lungs through the pulmonary arteries. These blood vessels can have diseases, as well.
- Pulmonary embolism (PE). A blood clot (usually in a deep leg vein, called deep vein thrombosis) breaks off, travels to your heart, and gets pumped into your lungs. The clot sticks in a pulmonary artery, often causing shortness of breath and low blood oxygen levels.
- Pulmonary hypertension. Many conditions can cause high blood pressure in your pulmonary arteries. This can lead to shortness of breath and chest pain. If your doctor cannot find a cause, they will call it idiopathic pulmonary arterial hypertension.
How Smoking Affects the Lungs
Cigarette smoking is the number one risk factor for lung cancer. In the United States, cigarette smoking is linked to about 80% to 90% of lung cancer deaths. Using other tobacco products such as cigars or pipes also increases the risk of lung cancer. Tobacco smoke is a toxic mix of more than 7,000 chemicals. Many are poisons. At least 70 are known to cause cancer in humans.
People who smoke cigarettes are 15 to 30 times more likely to get lung cancer or die from lung cancer than people who do not smoke. Even smoking a few cigarettes a day or smoking occasionally increases the risk of lung cancer. People who quit smoking have a lower risk of lung cancer than if they had continued to smoke, but their risk is higher than those who have never smoked. Quitting smoking at any age can lower the risk of lung cancer.
Many smokers have opted to switch to vaping with electronic cigarettes or e-cigarettes. E-cigarettes put nicotine into your lungs and bloodstream without the smoke and tar of a regular cigarette.
However, other harmful substances can get into your body when you vape, especially if you use flavoured cigarettes. E-cigarettes run on batteries and heat up nicotine, flavourings, and other chemicals. They turn them into a vapour you can breathe in. Many chemicals that cause cancer are in this vapour. That includes formaldehyde, heavy metals, and particles that can get stuck in the deepest parts of your lungs.
It is hard to know how much of these chemicals you breathe in when you vape. The levels are usually lower in e-cigarettes than regular cigarettes. But some studies show that high-voltage e-cigarettes have more formaldehyde and other toxins than standard e-cigarettes. Some chemicals in e-cigarettes can irritate the airways in your lungs and cause inflammation of lungs.
Covid-19 and Your Lungs
SARS-CoV-2, the virus that causes Covid-19, is part of the coronavirus family. Covid-19 is a respiratory disease which involves your lungs.
Covid-19 can cause a range of breathing problems, from mild to critical. Older adults and people who have other health conditions like heart disease, cancer, and diabetes may have more severe symptoms.
When the virus gets in your body, it comes into contact with the mucous membranes that line your nose, mouth, and eyes. The virus enters a healthy cell and uses the cell to make new virus parts. It multiplies, and the new viruses infect nearby cells.
The new coronavirus can infect the upper or lower part of your respiratory tract. It travels down your airways, causing the lining to become irritated and inflamed. In some cases, the infection can reach down into your alveoli.
Covid-19 is a new condition, and scientists are learning more every day about what it can do to your lungs. They believe that the effects on your body are similar to those of two other coronavirus diseases, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
- Mild and Moderate Cases
About 80% of people who have Covid-19 get mild to moderate symptoms. You may have a dry cough or a sore throat. Some people have pneumonia, a lung infection in which the alveoli are inflamed. - Severe Cases
About 14% of Covid-19 cases are severe, with an infection that affects both lungs. As the swelling gets worse, your lungs fill with fluid and debris.
You might also have more severe pneumonia. The air sacs fill with mucus, fluid, and other cells that are trying to fight the infection. This can make it harder for your body to take in oxygen. You may have trouble breathing or feel short of breath. You may also breathe faster.
- Critical Cases
In critical Covid-19 — about 5% of total cases — the infection can damage the walls and linings of the air sacs in your lungs. As your body tries to fight it, your lungs become more inflamed and fill with fluid. This can make it harder for them to swap oxygen and carbon dioxide.
You might have severe pneumonia or acute respiratory distress syndrome (ARDS). In the most critical cases, your lungs need help from a machine called a ventilator to do their job. There is evidence that 20-30% of critically ill patients can develop clots in the lungs, heart, brain, and legs, some of which are life-threatening. A few people have needed lung transplants because of severe tissue damage from Covid-19.
- Covid-19 Complications
It can take time to feel better after you have pneumonia. You may feel more tired than usual for a while. You might also find that you can’t exercise like you used to.
Some people have a cough even after they recover from Covid-19. Others have scarring in their lungs. Doctors are still studying whether these effects are permanent or might heal over time.
Taking Care of Your Lungs
Sometimes, we take our lungs for granted. They keep us alive and well, and for the most part, we don’t need to think about them. That is why it is crucial to prioritize your lung health.
Your body has a natural defence system designed to protect the lungs, keeping dirt and germs at bay. Here are some ways to keep your lungs healthy.
- Stop smoking and stay away from second-hand smoke.
- Avoid indoor and outdoor air pollution.
- Avoid exposure to people who have the flu or other viral infections.
- Exercise regularly.
- Eat a healthy, balanced diet.
- Maintain a healthy weight.
- See your doctor for an annual physical.
 Article by Dr. Malwinder Singh Sandhu
Article by Dr. Malwinder Singh Sandhu
Resident Clinical (Medical & Radiation) Oncologist
Sri Kota Specialist Medical Centre


