There are two major types of skin cancers: melanoma and non-melanomatous skin cancers. According to Malaysia’s National Cancer Registry, skin cancers account for 2.6% of all malignancies and is the 10th most common malignancy in the country (Third National Cancer Registry Report 2003-2005).
Melanoma is probably the most serious form of skin cancer. Survival rates depend on the stage of the disease at the time of presentation, and therefore early diagnosis is crucial to improve patient outcome. Patients themselves may detect these lesions; detection by a clinician however is usually associated with a thinner and more curable cancer.
Most melanomas are superficial that are confined to the epidermis layer of the skin and they can remain for months to years. During this ‘horizontal’ growth phase the disease can be cured in most cases with surgical excision alone.
Once the disease spreads into the dermis it will demonstrate a ‘vertical’ growth phase and harbours metastatic potential. The measurement of the thickness of the tumour (known as the Breslow depth) is strongly associated with the probability of metastases.
Classically there are four major morphological subtypes of melanoma: superficial spreading melanoma, nodular melanoma, lentigo maligna melanoma, and acral lentiginous melanoma.
Acral lentiginous melanoma accounts for less than 5% of all melanomas; however it is the most common form of melanoma seen in darker pigmented individuals. These melanomas occur in the palms, soles and underneath nail plates (subungual).
The clinical diagnosis of melanoma can sometimes be challenging. There are several questions that can be asked regarding any suspicious looking skin lesion (naevi) such as:
- When was the lesion first noticed?
- Has the lesion changed in size, shape, colour, and/or symptoms (eg, bleeding, itch)?
- Is there a personal or family history of melanoma?
- Were they any severe sunburns during childhood or teenage years?
- Is there a history of excessive sun exposure?
- Does the patient have a cancer-prone syndrome (eg, familial atypical mole and melanoma syndrome or xeroderma pigmentosum)?
- Were there any previous exposure to psoralen plus ultraviolet A (PUVA) therapy?
- Is the patient immunosuppressed?
The ABCDE rule first coined by dermatologists from New York University was devised to help clinicians and laypeople to help identify early melanoma:
A: Asymmetry
B: Border irregularities
C: Colour
D: Diameter (>6 mm)
E: Evolution (change colour, shape, size over time)
The definitive diagnosis of melanoma requires histo-pathological confirmation i.e a biopsy. Ideally this should be done by a trained health care professional, e.g. a trained dermatologist.
Once melanoma is confirmed, patients should be counseled regarding their treatment options ideally by a multidisciplinary team that should include a surgeon, a dermatologist and a medical oncologist +/- radiation oncologist.
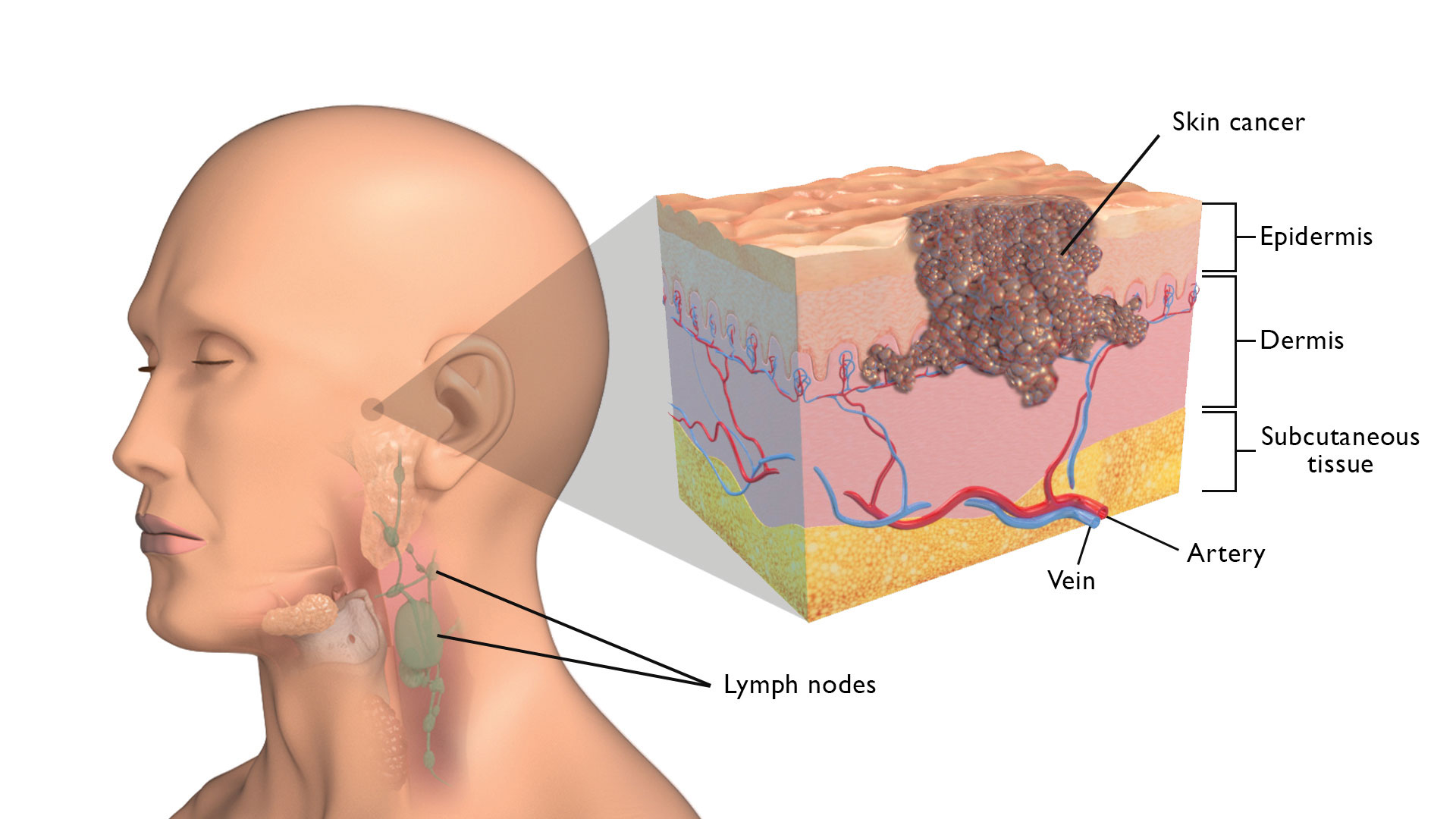
Surgically, a wide local excision with adequate normal tissue margins is required. The width of normal tissue to resect melanomas arising from the trunk or extremities is based on the thickness of the primary tumor. As melanomas can spread along lymphatic channels, surgical staging of local-regional draining lymph nodes may be required depending on the risk of spread from the primary tumour.
Patients who present with early stage disease may not require adjuvant (post-operative) treatment. However patients with higher risk disease (for e.g. stage III disease with lymph node involvement) should have a discussion with an oncologist regarding the role of adjuvant systemic treatment.
The advent of immunotherapies and targeted agents has changed the treatment landscape for patients with melanoma. For e.g. adjuvant immunotherapy (for e.g. PD-1 inhibitors) could be offered for a year for most patients with stage III disease and can extend their disease free-survival rates.
These treatment advances have changed patient outcomes over the last few years who have disseminated (metastatic) disease compared to conventional therapies. Examples of such treatments include Immunotherapy (IO with checkpoint inhibition) and MAP (mitogen-activated protein) kinase pathway inhibitors.
Immunotherapy treatment helps to initiate an anti-tumor immune response directed against melanoma. This can be associated with a variety of autoimmune side effects however and will require monitoring and management under an oncologist. Certain patients with disseminated melanoma whose tumours harbour a BRAF V600E mutation (present in 40-60% of metastatic melanomas) could also benefit from BRAF and MEK inhibitors.
In conclusion it’s important to seek the advice and dermatological opinion for any skin lesions that may appear suspicious so that a timely diagnosis and appropriate treatment can be initiated, as early diagnosis can save lives.
 Dr Abel Zachariah
Dr Abel Zachariah
Consultant Clinical Oncologist,
Pantai Hospital Ayer Keroh


