Peripheral arterial disease or PAD is a common circulatory problem that limits the blood flow to your limbs. One of the symptoms of such a disease is a pain in your legs when walking.
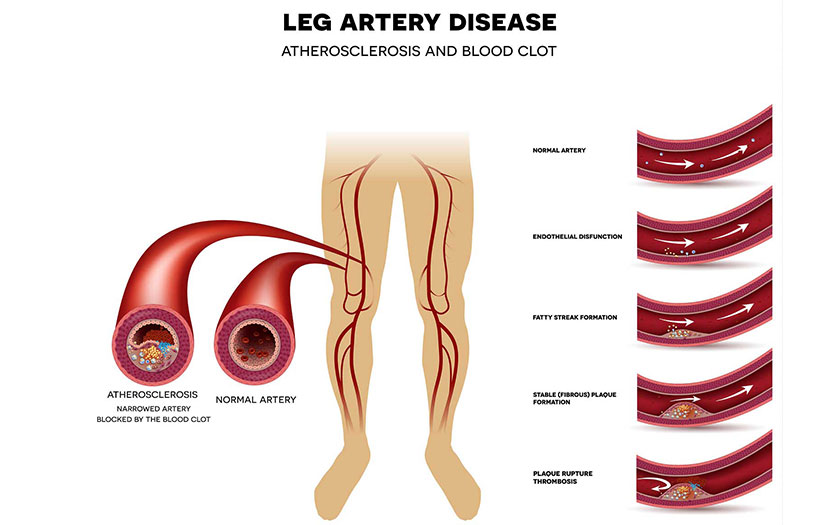
This disease is often caused by atherosclerosis. In atherosclerosis, fatty deposits (plaques) build up in your arterial walls and reduce blood flow.
While this situation is common with the heart, this could also cause a problem in the lower limbs when blood flow is restricted in certain areas. People who suffer from diabetes, hypertension, and high cholesterol has a higher risk of developing atherosclerosis.
How would it affect you?
PAD affects not only how well you live but also how long you may live. You may find that that you can’t walk as far or for as long as you used to—and that’s frustrating—but if you have PAD, you are also at greater risk for having a heart attack and stroke
Approximately 160,000 to 180,000 of the estimated 18 million Americans with PAD will undergo a limb amputation as a result of PAD-related condition this year, resulting in lower quality of life, high medical costs, and shorter life expectancy.
Signs and symptoms
While most of the patients with PAD have mild or no symptoms, some may have leg pain when walking (claudication). Some of the common symptoms may include painful cramps in your hip, thigh or calf muscles after certain activities, such as walking or climbing the stairs. You may also experience hair loss or slower hair growth on your legs.
The legs may have a weak pulse or no pulse at all. Either foot could feel cold, darken or change colour. Furthermore, there can be sores or ulcers on your toes, feet or legs that won’t heal; these are diabetic foot ulcers. In men, a symptom of PAD could also be erectile dysfunction.
Peripheral Arterial Disease (PAD) can cause claudification, which is fatigue or heaviness in the leg muscles. These muscles affect the thighs, calves, and buttocks. People experiencing this symptom may have a hard time walking, climbing stairs, riding a bike, or performing other activities.
Complications
Failure to recognize and treat the disease may likely result in serious consequences such as Critical Limb Ischemia (CLI), which may result in gangrene, possibly requiring amputation of the affected limb. It could also result in sepsis – non-healing ulcers especially in diabetics who are more prone to infection.
Diagnosis
When you experience some of the symptoms, your doctor may perform the following tests to confirm the diagnosis: ankle-brachial index, duplex ultrasound, CT angiography, and invasive angiography.
Treatment Options
There are two main objectives in treating peripheral arterial disease. Firstly, to manage the symptoms by increasing blood flow to the affected limb. This will reduce the progression of gangrene thus salvaging the limb from the risk of amputation. Secondly, to stop the progression of atherosclerosis throughout the body to reduce risks of heart attack and stroke.
Depending on the severity of your condition, your doctor may initiate medications to optimize blood sugar, blood pressure, and cholesterol control. He may also recommend angioplasty, an invasive procedure whereby a balloon and/or stent is inserted into the blood vessel to restore blood flow to the affected limb. Last of all is the option of a bypass surgery which is open surgery to create a graft bypass to the occluded/narrowed blood vessel.
DID YOU KNOW?
If you have PAD, you’re more likely to also have ischemic heart disease, heart attack, stroke, and transient ischemic attack (“mini-stroke”). Talk to your doctor on how to control P.A.D. and lower your risk for these other conditions.
Source: https://www.nhlbi.nih.gov/health-topics/peripheral-artery-disease
 Dr Alan Koay Choon Chern
Dr Alan Koay Choon Chern
Consultant Interventional Cardiologist
Columbia Asia Hospital-Taiping


