Getting to know your pancreas is important. This organ is rarely discussed amongst friends and families as the organ is hidden deep in the tummy and when it gets sick, it mimics other diseases like “gastric pain.”
When one has severe gastric or tummy pain, it is important to seek medical attention. The first thing to consider is maybe a heart attack if one is at risk of it. On the other hand, pancreatitis must also be part of the consideration when dealing with severe upper tummy pain. Let’s have a closer look at the role of our pancreas and get a better understanding of pancreatitis.
THE ROLE AND FUNCTION OF OUR PANCREAS
There are two main functions of pancreas. First, it is the main organ that secretes insulin. When the insulin secretion is inadequate, it leads to diabetes mellitus. Secondly, it secretes digestive juices to help protein and fat digestion.
If the second function is lost, a person will have maldigestion which will manifest as weight loss and diarrhoea with stool that floats above water. When fat content in the stool increases, stool will become lighter than the water and thus, floats to the surface. In medical team we called this steatorrhea.
WHAT IS PANCREATITIS
Pancreatitis is a condition where the pancreas is injured (by an insult) and causes common reaction of injury such as pain, swelling, redness and maybe loss of its function.
There are two types of pancreatitis: Firstly, acute pancreatitis which occurs over a few hours and manifests as sudden severe pain at the upper tummy. The second type is chronic pancreatitis which occurs over a span of months to years. It manifests gradually over time with dull tummy ache, loss of weight and steatorrhea, as well as diabetes mellitus.
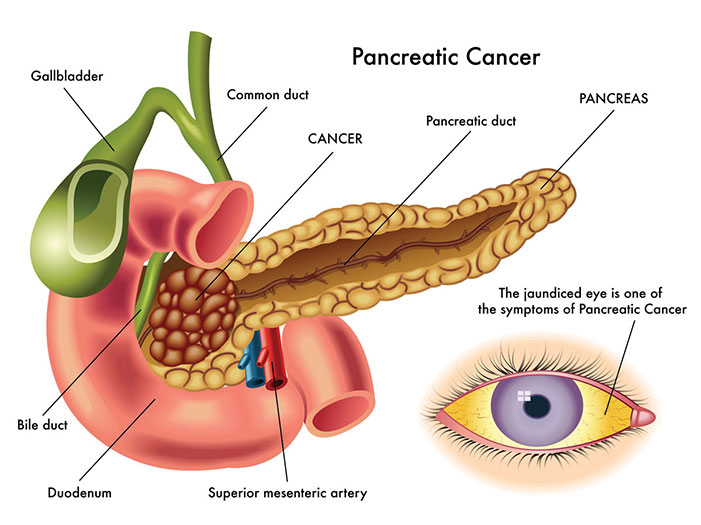
Acute pancreatitis in Malaysia is frequently related to transient blockage of small stones that usually originate from the gallbladder. This blockage causes the backflow of the pancreatic juice and the juice’s enzyme activation. This in turn digests the pancreas itself rather than food and leads to severe pain.
It is important to note that not all patients who have gallstone will have pancreatitis. It is those patients who have had a gallstone and pancreatitis that are at high risk – around a third of them will recur. For these patients, we suggest investigating and removing the gallbladder to prevent future sickness.
Other causes including (but not limited to) toxic injury from heavy alcohol use or binging, some poison from scorpions and although rare, certain medications. Of note, extremely high triglyceride – one of the cholesterols in the blood stream, may lead to this condition too.
As for chronic pancreatitis, the most common cause is still chronic use of alcohol and smoking cigarettes. Other rare causes include the body’s own antibody attacking the pancreas slowly which may result in the organ’s malfunction.
Signs and symptoms of pancreatitis
The main symptom of acute pancreatitis is extreme pain in your tummy. It occurs suddenly and increases to maximum pain within 30 minutes. This pain is usually not tolerable. The pain can spread to the left side of abdomen, or the whole abdominal region and even to the back. Patients frequently think that this is merely “gastric pain” – until it is not tolerable. Usually at this point, they will proceed to seek medical attention.
As for chronic pancreatitis, the symptoms are very subtle. It usually starts with loss of appetite and weight, then diarrhoea with higher fat content in stool or steatorrhea. It may be accompanied with a dull ache over the upper part of tummy. It may also be confused as cancer initially as the symptoms are quite similar.
SEVERE COMPLICATIONS
Acute pancreatitis may lead to kidney, heart and vessel, as well as lung failure in the initial phase. If the pancreas is severely damaged, the patient may later have diabetes mellitus. It is not uncommon that after the initial phase of pancreatitis, the fluid and tissue that died off (necrosis) may form a collection of fluid around that region which occasionally needs special endoscopic or radiology skills to drain the fluid. Having surgery to handle this situation is sometimes required but the need to do that has become lesser with the advancement of other treatments available today.
As for chronic pancreatitis, the main complications include diabetes mellitus which usually requires insulin treatment. People in this condition are at risk of malnutrition, especially if they are using alcohol and have lack of enzyme to digest protein and fat. Chronic pancreatitis is also predisposed to pancreas cancer, a deadly cancer which is difficult to detect.
Avoidance of alcohol and cigarette use seems to be the logical way to prevent pancreatitis. Also, getting treatment for gallstone disease, including surgery to remove the gallbladder, if there is already a gallstone-related pancreatitis. Follow doctors’ advice if you are having familial disease of extremely high triglyceride type of cholesterol-related disease. You will need special medication control for the triglyceride level.
 Article by Dr. Gew Lai Teck
Article by Dr. Gew Lai Teck
Visiting Gastroenterologist and Hepatologist
Sri Kota Medical Centre


