Telemedicine was originally intended as a method to treat patients in remote locations, who were situated far away from healthcare facilities or professionals.
While it is still used today to address such problems, it has become a tool for convenience. Patients today turn to telehealth for immediate treatment to avoid the hassle of travelling down to the clinics and spending time in the waiting room.
Commercial payors support telehealth due to potential lower costs from lower drug mark-ups and lower expenses incurred, especially for patients located in rural areas, due to episodes of care whereby virtual appointments can replace physical appointments. Providers also appreciate the higher efficiency resulting from quicker diagnosis and treatments arising out of telemedicine.
The Covid-19 pandemic also sped up the adoption of telehealth since physical consultations were restricted and this helped reduce the risk of infection.
Roland Berger’s latest study, “Telehealth 2.0: Expanding the reach of healthcare in the Asia Pacific” explores today’s telehealth systems’ challenges and opportunities using Orthopedics as a focal example.
Challenges and limitations of today’s telehealth systems
The study raised three challenges and limitations of today’s telehealth systems. Operating solely on an episode-based model amplifies that telehealth is not a one size fits all solution. The telehealth models are currently built for acute episodic care and may not be effective on patients that require constant reviews and chronic care, such as ageing societies.
Teleconsultations are also not able to deliver the best results without physical examinations and updated images. In almost 20% of the Orthopedic cases, physicians had expressed a need for physical examination follow-ups to assess several motor tests more accurately. A lack of centralized access to imaging repositories also delayed accessibility to patients’ records.
More efforts need to be invested in infrastructure development for telehealth systems in Asia Pacific. Various markets are underserved and suffering from a shortage of diagnostic facilities such as the DEXA scan machines, which help detect bone disorders. It is also crucial to obtain the buy-in of telemedicine from sceptical key decision-makers and renowned doctors, as they can influence patients to adopt telemedicine. Addressing and resolving the risks such as the potential loss of data or incorrect data input may help to change their mindsets.
Evolving systems and roles to work hand in hand
In order to advance telemedicine from a service to an ecosystem enabler, the roles of the healthcare stakeholders and system would need to evolve and keep up with today’s challenges.
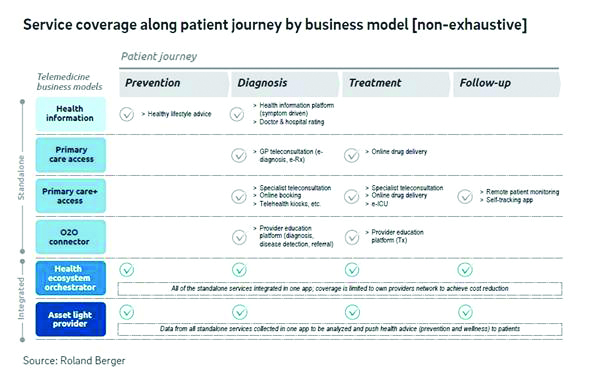
Six telemedicine business model platforms were identified in Southeast Asia, namely – Health Information, Primary Care Access, Primary Care+ Access, Organization- to-Organization Connector, Health Ecosystem Orchestrator and Asset-light Healthcare Provider.
Popular model archetypes implemented in Asia Pacific include the Primary Care+ Access, a platform that provides an amplified care model. In addition to GP services, they provide referrals / assistance with patient’s access to tertiary care including diagnostic centers, specialty care providers, hospitals, rehabilitation centres and pharmacies. The platform in most cases, however, does not have full integration with rest of the healthcare stakeholders.
An integrated option is the Health Ecosystem Orchestrator, a telemedicine model which coordinates more complex interactions and transactions between patients, providers, payors and other healthcare stakeholders. The orchestrator usually enables care by going beyond the traditional channels and partnering with adjacent players who have stakes in a healthier population like banks, telecoms and retail. Due to its integrated and seamless interface, the Orchestrator model stood out as the recommended way forward for Southeast Asia.
This model also ensures affordable healthcare for the community by keeping patients within the network and removing redundancies.
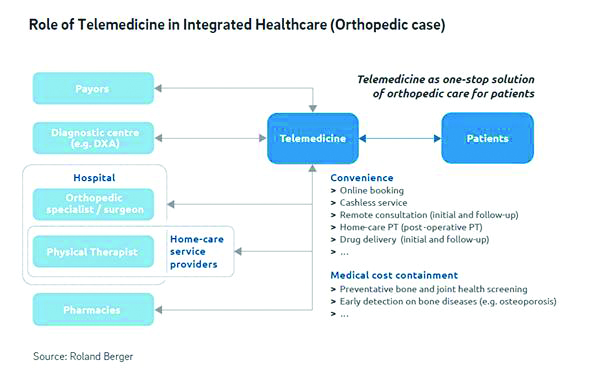
Through the Orchestrator model, telemedicine can integrate several facilities in one platform such as payors, diagnostic centers, hospitals, home-care service providers and pharmacies. Services such as insurance claims, follow-up consultations or drug deliveries are all easily accessible and arranged via one platform. The challenges of standalone models can be mitigated. Developing payor led incentives and wellness programs would also become easier due to lower constraints of brand positioning and operating model flexibility. “Through simulations and observations using the Orchestrator model, the average waiting time can be reduced 50-70% and doctor capacity increased by 20-25%”, says Mr Yoshihiro Suwa, partner and co-author of the study.
For the ideal telemedicine platform to run smoothly, this would also require stakeholders to transit towards supporting the digital transformation of the healthcare system.
Policy makers and regulators should develop supporting policies to enable telemedicine and define standards and protocols to help reduce inefficiencies at a broader scale for equitable healthcare.
Healthcare providers should seize the opportunity with instituting synchronous models and invest in infrastructure for a seamless online to offline integration.
Payors with incentive linked programs can significantly influence patient’s behaviour on choosing preventative care and wellness. Health insurers can digitally steer their customers toward a network of preferred partners.
Tech startups and medical tech firms’ collaborations enable telemedicine to provide more value-added services to patients with less capital and technology investment. This can help drive access and care in unwanted markets.
Pharmaceutical companies can drive patient and healthcare professional engagement at scale and adopt strategies to go beyond the pill, such as utilizing data on medical research and development for new treatments.
As the hype cycle of telemedicine in Asia Pacific begins to taper, business models in the space would have to evolve towards value addition beyond remote care consultation.
“Given the fragmented nature of healthcare delivery in some of the emerging markets of Asia Pacific, telemedicine models of the future could aim to bring the various parts of the value chain under one virtual roof”, states Mr Aditya Agarwal, principal and co-author of the study. Should they succeed, they shall bring tremendous efficiencies for healthcare systems already reeling under budgetary pressures.
Co-author of study: Aditya Agarwal


